|
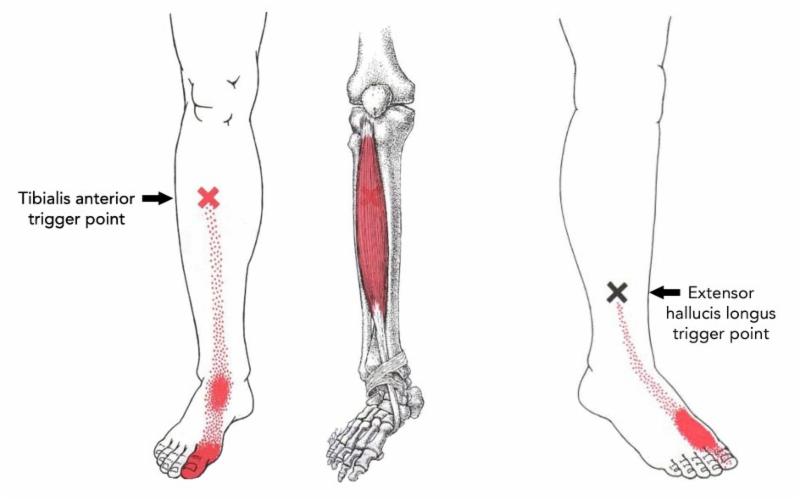
Dear Colleagues: Last month's newsletter included three English-language articles on neural therapy. I hope you found time to read them or at least place them on your desktop to be read later. This month I intend to get back to the usual format of something short and quick that can be easily applied to medical practice. The subject? - a painful big toe. I suppose the first thing that comes to mind when a patient presents with a painful big toe is gout - that is, assuming there is no history of trauma. When the gouty attack is full-blown, diagnosis is usually simple - a red, painful, exquisitely sensitive toe, with pain exacerbated by active or passive joint movement. When less acute, diagnosis can be problematic, as the pattern is similar to any other form of toe arthritis. An elevated serum uric acid usually makes the situation clear. If the onset of pain was preceded by trauma, traumatic arthritis, subungual hematoma, ligament strain or fractures need to be ruled out. All of these will display local symptoms and signs when examined carefully. Where diagnosis becomes more challenging is when minimal signs of tenderness, swelling or pain on movement are present. Then we must start thinking about referred pain. (Some tenderness may be present with referred pain.) Elementary neuroanatomy tells us that irritation of a L5 nerve root can cause pain in a first toe, although it is usually accompanied by pain down the posterior leg. An uncommon cause of first toe pain is pain referred from the liver through the corresponding acupuncture meridian. The liver meridian extends down to the lateral side of the first toe. One method of diagnosing is checking the liver by autonomic response testing. Treatment may be neural therapy of the liver. Pain can also be referred from musculoskeletal structures. A quick check of Hackett's map of referred pain from low back ligaments shows no referral of pain to the first toe. However pain can be referred to the first toe from hip ligaments. And then there are muscles, in particular, their trigger points. I personally have been unable to memorize all the pain referral patterns from muscle trigger points, so I depend on Travell and Simon's 2-volume "Myofascial pain and dysfunction: The trigger point manual". Not only are these books well written and well illustrated but also the organization is superb. The first volume is about the upper part of the body, the second the lower. In the inside of the front cover is a list of the muscles in the volume and on the facing page a guide to where they can be found. In the case of toe pain, we are quickly directed (in the second book) to Chapter 18 where one finds that great toe pain can be referred from three different muscles: the tibialis anterior, the extensor hallucis longus and the flexor hallucis brevis. Each pattern is somewhat different, e.g. the tibialis anterior trigger point (TP) also refers to the anterior ankle. The extensor hallucis longus referral pattern does not include the anterior ankle, but centers more on the dorsal aspect of proximal first toe.
Examination including muscle strength can give clues, but ultimately the TP has to be found in the muscle. When it is found an injection of procaine ½% into the TP combined with stretching the muscle can give relief from the toe pain. Alternatively, the Travell "spray and stretch" technique can be used or the TP can be treated directly with an energetic device such as the Tenscam. The patient who reminded me of this was an otherwise healthy 70-year old man who presented with pain over the proximal first toe. He gave no history of trauma or strain. He felt it most while walking, especially during the weight-bearing phase of gait. A trigger point was detected distal to the junction of the medial and lower thirds of the lower leg, anterior to the fibula. Travel and Simons always give advice about "perpetuating factors", those conditions that give rise to TPs in the first place. To these, the neural therapist can add the possibility of other interference fields and the osteopath can search for somatic dysfunction. In the patient mentioned above, a tight piriformis muscle was present, probably related to chronic sacroiliac instability. In the case of toe pain from tibialis anterior or extensor hallucis longus trigger points, the leg and pelvis should be searched for interference fields in scars, in old bone contusions, in injection sites and in the L3 sympathetic ganglion. Identification and treatment of trigger points is an important part of neural therapy and often helps solve difficult-to diagnose pain problems. But the neural therapist should not stop at simply treating the TP. The factors that created the TP should be addressed as well as associated interference fields. |
|
A free Spanish language neural therapy newsletter is available, published by D. David Vinjes of Barcelona, Spain at http://www.terapianeural.com/. Sign up at the site! Discussions are underway with regard to translating both English and Spanish literature. Feedback with regard to interest is invited from you, the readership of this newsletter. Your feedback is always welcome. |
| Contact Information
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~ email: drkidd@neuraltherapybook.comphone: 613-432-6596 web: http://www.neuraltherapybook.com ~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~ |